Publications and Other Healthcare Materials
Accelerated speed to market begins with research and collaboration
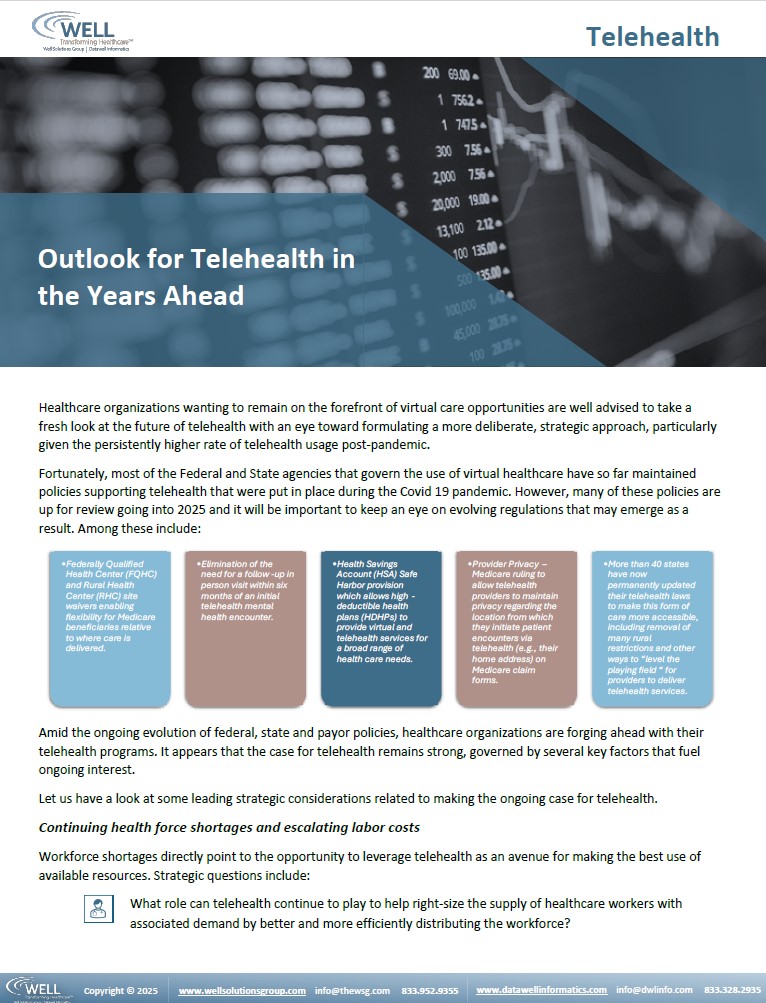
Telehealth
Outlook for Telehealth in the Years Ahead
Healthcare organizations wanting to remain on the forefront of virtual care opportunities are well advised to take a fresh look at the future of telehealth with an eye toward formulating a more deliberate, strategic approach, particularly given the persistently higher rate of telehealth usage post-pandemic.
Medicaid Changes and Challenges for Health Plans
There are both immediate and longer-term changes that set forth an uncertain and multi-dimensional framework for health plans and provider organizations to consider as they think about individuals served and ways to plan for and/or mitigate the health care consequences for the diverse groups of individuals served who may be at risk.
Combatting Fraud in Healthcare Billing and Payment
Fraud in healthcare billing and payment continues to be a serious risk for payers and providers alike. Billions of dollars are misappropriated every year resulting in increasing costs throughout the healthcare delivery system.
Public and private payers are serious about rooting out fraud, waste, and abuse in the health care system wherever it may occur, given the magnitude of the problem.
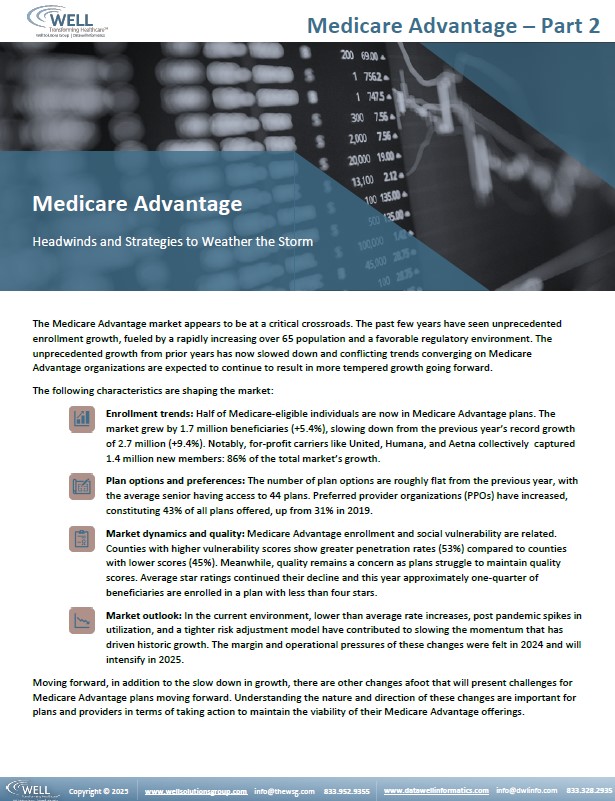
Medicare Advantage – Part 2
Headwinds and Strategies to Weather the Storm
The Medicare Advantage market appears to be at a critical crossroads. The past few years have seen unprecedented enrollment growth, fueled by a rapidly increasing over 65 population and a favorable regulatory environment. The unprecedented growth from prior years has now slowed down and conflicting trends converging on Medicare Advantage organizations are expected to continue to result in more tempered growth going forward.
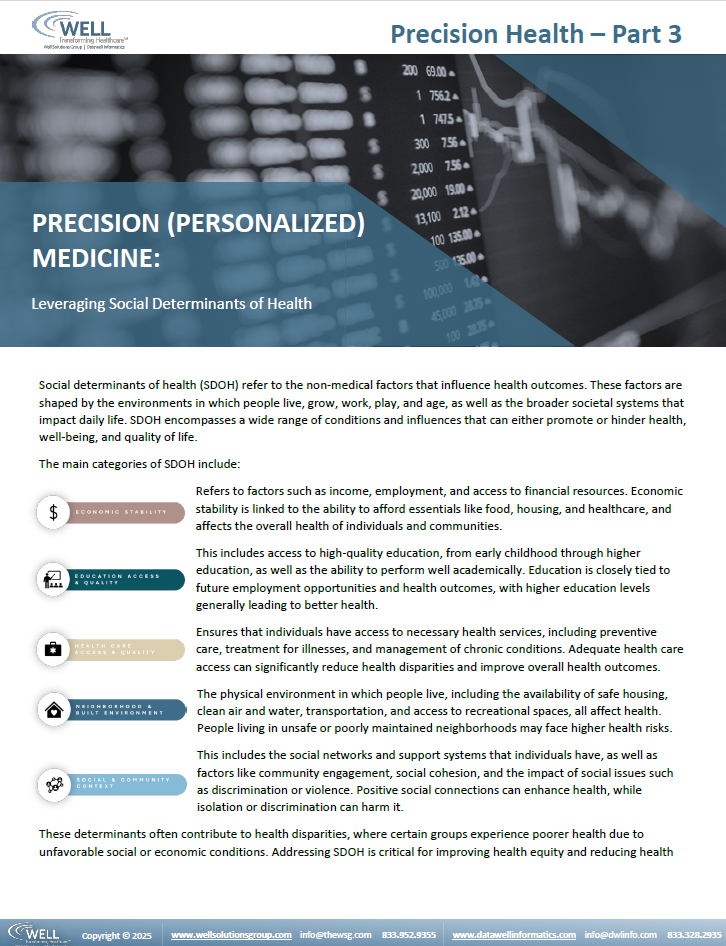
Precision Medicine – Part 3 – February 2025
Leveraging Social Determinants of Health
Social determinants of health (SDOH) refer to the non-medical factors that influence health outcomes. These factors are shaped by the environments in which people live, grow, work, play, and age, as well as the broader societal systems that impact daily life. SDOH encompasses a wide range of conditions and influences that can either promote or hinder health, well-being, and quality of life.
These determinants often contribute to health disparities, where certain groups experience poorer health due to unfavorable social or economic conditions. Addressing SDOH is critical for improving health equity and reducing health disparities across populations. Programs and policies aimed at improving SDOH, such as increasing access to education, healthcare, and economic resources are essential for fostering better health outcomes for all.
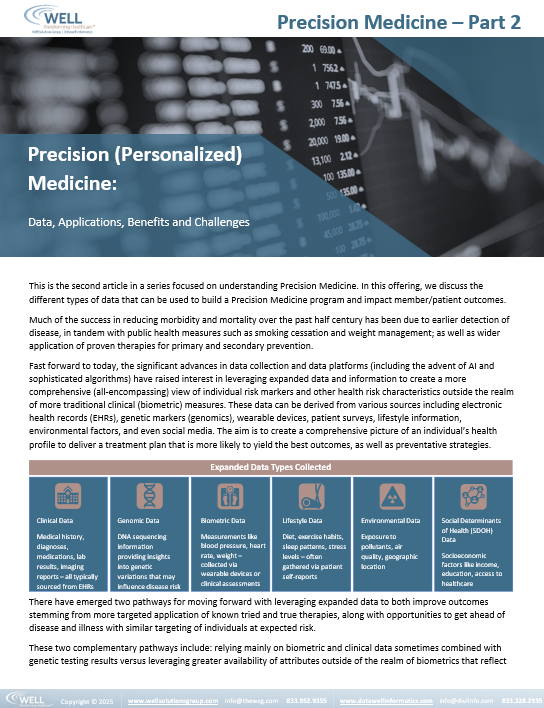
Precision Medicine – Part 2 – January 2025
Data, Applications, Benefits and Challenges
Much of the success in reducing morbidity and mortality over the past half century has been due to earlier detection of disease, in tandem with public health measures such as smoking cessation and weight management; as well as wider application of proven therapies for primary and secondary prevention.
Fast forward to today, the significant advances in data collection and data platforms (including the advent of AI and sophisticated algorithms) have raised interest in leveraging expanded data and information to create a more comprehensive (all-encompassing) view of individual risk markers and other health risk characteristics outside the realm of more traditional clinical (biometric) measures.
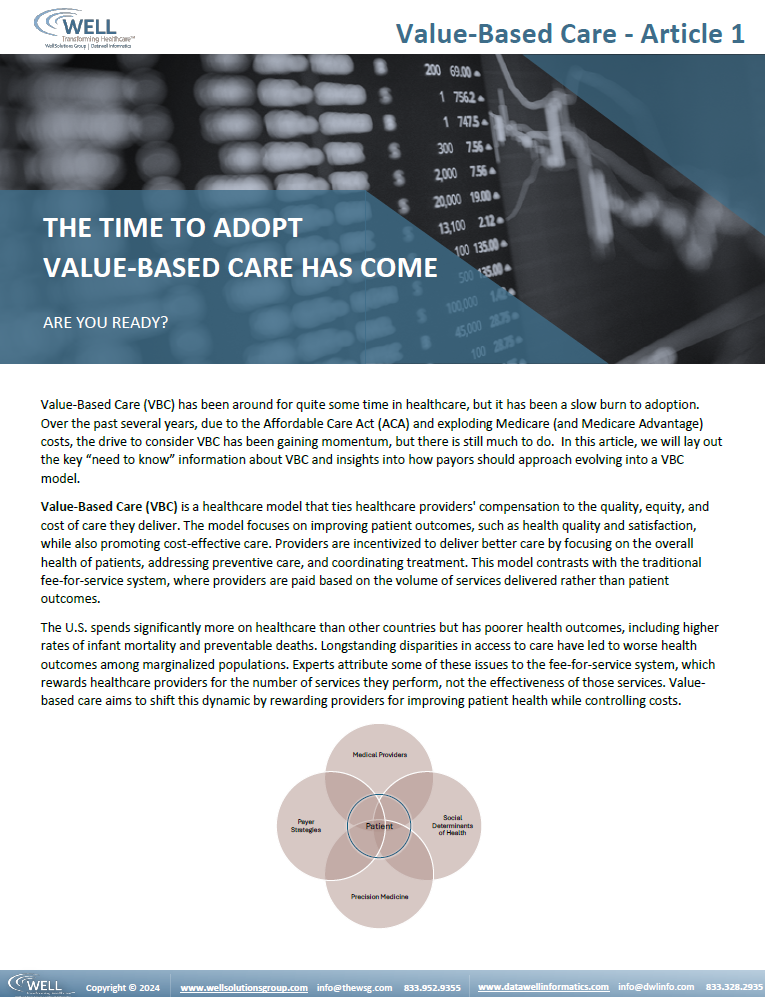
Value-Based Care – Article 1 – December 2024
Value-Based Care (VBC) is a healthcare model that ties healthcare providers’ compensation to the quality, equity, and cost of care they deliver. The model focuses on improving patient outcomes, such as health quality and satisfaction, while also promoting cost-effective care. Providers are incentivized to deliver better care by focusing on the overall health of patients, addressing preventive care, and coordinating treatment. This model contrasts with the traditional fee-for-service system, where providers are paid based on the volume of services delivered rather than patient outcomes.
CMS Pre-Authorizations – November 2024
CMS Interoperability and Prior Authorization Final Rule Synopsis
The Centers for Medicare & Medicaid Services (CMS) changed its prior authorization rules to simplify and digitize the process, and to reduce the burden on each of the three legs in the healthcare delivery tripod: patients, providers, and payers. In particular, CMS aims to reduce administration, simplify and accelerate the process, and introduce standardization across payers.
It is critically important for providers and especially payers to get ahead of these changes by assessing processes and the technology necessary to support the rules change and ensure compliance.
Precision Medicine – Part 1 – September 2024
Precision Medicine as key driver of next generation personalized health care
The term “Precision Medicine” refers to the tailoring of clinical and other health care-related interventions based upon an individual’s unique make-up and circumstances. While personalization of care has long been the underpinning of best practice medicine, personalized care and Precision Medicine are not exactly synonymous. Precision Medicine is an expanded approach that uses information about an individual’s biological, environmental, and lifestyle characteristics to guide decisions related to their medical and health management.
Medicare Advantage – Planning for the Future – Part 1 – July 2024
Part 1: The Current Landscape
The remarkable growth in Medicare Advantage enrollment over the past twelve years is raising questions about both the cost and quality of that coverage as well as the ultimate impact on health equity and solvency of the traditional Medicare program.
This is the first in a series of articles to follow, providing insight into the current landscape (both in terms of Medicare Advantage performance and growth) to help lay the foundation for steps that plan sponsors and provider organizations can be taking to prepare for the future.
Payment Integrity 101 – Article 3 – June 2024
Payment Integrity Evolution
Over the past decade, the healthcare industry has seen payment integrity evolve from an under-resourced operational niche to a strategic asset that is central to the overall management of medical expense. A paradigm shift is underway, wherein many payers are recognizing that the status quo will not suffice in a volatile, disruptive market where, among other things, technology is advancing rapidly. Many are at the initial stages of fully understanding and implementing elements of a comprehensive future vision for payment integrity efforts, which in addition to dedicated analytic staff, comprise a team committed to ideation and innovation. Vital measures to track and drive performance of Payment Integrity (PI) initiatives, including the use of industry benchmarks and annual goal setting are gaining traction.
Payment Integrity 101 – Article 2 – June 2024
Guiding Principles: Payment Integrity as a Strategic Enterprise Solution
Today’s technology innovations and workforce challenges (need to drive toward greater efficiency) are prompting payers to take a closer look at payment integrity with an eye toward a more strategic framework. More and more payers are recognizing that the status quo will not suffice in a volatile, disruptive market where change is happening with increasing speed.
Over the past decade, the healthcare industry has seen payment integrity evolve from an under-resourced operational niche to a strategic asset that is central to the overall management of medical expense, in addition to efforts to improve quality of care and foster mutually satisfying provider relations. Let’s look at some guiding principles establishing Payment Integrity as a strategic asset.
Payment Integrity 101 – Article 1 – May 2024
Current State of Healthcare Payment Integrity: Article 1
Understanding what healthcare payment integrity entails and why there is renewed interest
Payment integrity encompasses efforts on the part of payers and healthcare providers alike to navigate ongoing challenges relative to achieving accurate and efficient payment. Having a system of payment integrity processes in place is essential for ensuring financial accuracy, maintaining compliance with regulators, optimizing the overall healthcare delivery system, and removing administrative waste which can have a negative impact on patient care and quality outcomes.
WEBINAR: DataWELL CISO, Robin Smith Joins Panel on Elevating Women in Compliance & Technology
Women in Compliance & Technology
March is Women’s History Month, and while we should be celebrating female leaders in our industries every day, it offers a good opportunity for those of us in the tech space to take stock of the incredible women leading the charge in the industry and appreciate how far they’ve come.
AI: Healthcare Data Privacy & Security – March 2024
Harnessing the Value of Artificial Intelligence (AI):
Protecting healthcare data privacy and security
AI at its core encompasses taking advantage of the rich and diverse sources of information that individuals and health care providers amass across the continuum of health-related behaviors, interactions, and management. Being able to better leverage these stores of data to enable predictions of health risk and more proactive engagement to promote better health care outcomes via AI tools and applications offers great promise. With this comes a responsibility to safeguard and ensure responsible stewardship of sensitive information. This includes both the use of the data itself as well as the output, predictions and actions that ensue.
Successful Process Improvement Management – February 2024
Process Improvement: It Takes Leadership
How process improvement is managed above and beyond what is done is a key ingredient for success and can make the difference between a well-executed improved process and one that fails to deliver demonstrative, sustainable results.
Our view of process improvement success is less about the process and tools mechanics and more on sharing insights on the leadership of the process – what are the management principles that come into play when the goal is to identify, plan and execute a successful process improvement initiative?
As a backdrop to help illustrate this perspective, we will leverage a recent successful process improvement engagement undertaken on behalf of one of our clients. Let’s start there.
AI for Population Health Management – Article 1 – January 2024
AI Practical Uses and Understanding – Starting with the fundamentals
This is the first in our short series of articles about prospects for advancements in population health management (and health care overall) through the application of Artificial Intelligence (AI). Here we set out to provide a general overview and orientation on this topic, to be followed with subsequent article(s) delving further into how to get started with AI and suggested applications for practical and effective use.
The Evolution of Healthcare – Article 3 – November 2023
Mental & Physical Health
Paving the Way for Mind-Body Integrated Care
In this the third article in our series on Mental and Physical Health, we will delve further into describing some of the different modalities in use to address mental and physical health more holistically, emerging collaborative models, as well as existing barriers to adoption.
Health care organizations and physician practices that offer or plan to offer population health management services to patients will want to pay closer attention to opportunities associated with more holistic integration of care that takes into account the mind-body connection.
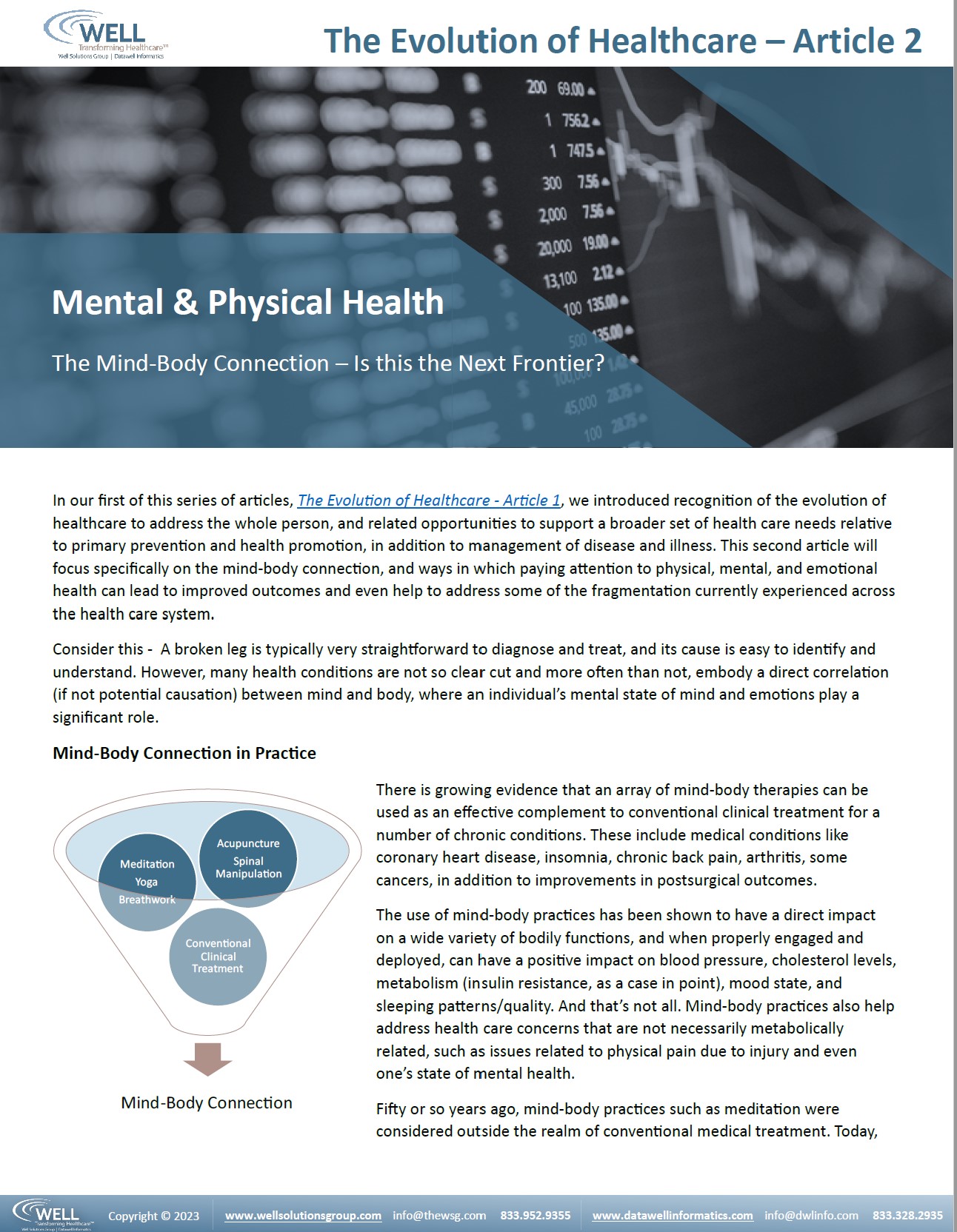
The Evolution of Healthcare – Article 2 – October 2023
Mental & Physical Health
The Mind-Body Connection – Is this the Next Frontier?
In our first of this series of articles, The Evolution of Healthcare – Article 1, we introduced recognition of the evolution of healthcare to address the whole person, and related opportunities to support a broader set of health care needs relative to primary prevention and health promotion, in addition to management of disease and illness. This second article will focus specifically on the mind-body connection, and ways in which paying attention to physical, mental, and emotional health can lead to improved outcomes and even help to address some of the fragmentation currently experienced across the health care system.
Analytics for Population Health Management – Article 5 – September 2023
Use of Expanded Data Sources for Program Outcomes and Evaluations
The challenge related to having the right data at the right time.
Development of population health programs is a key responsibility of population health managers and within a health plan setting, investments associated with these programs typically involve a large investment of time and resources. The scope of work to design health interventions can also become cross-functional as these programs will often impact operational processes, systems design, provider network contracting, staffing levels and pricing.
The Evolution of Healthcare – Article 1 – September 2023
Mental & Physical Health
Recognizing the importance of managing individuals’ health holistically via integration of mainstream and alternative care
Historically, health management programs have focused on one chronic disease at a time, often missing opportunities to support a broader set of health care needs related to primary prevention and health promotion. Those same programs had previously largely omitted an expanded focus to include social as well as mental health and emotional needs, via both traditional and non-traditional services. When building any population health programs, factoring in emotional well-being has not only proven to increase outcomes, but it improves the member experience. This article is the first in a series highlighting the evolution of U.S. Healthcare focus from primarily physical health symptomatic interventions to the entire person; and the opportunities that provides for enriched services and programs to improve outcomes.
Analytics for Population Health Management – Article 4 – July 2023
Expanding Data Sources for Identification of Risk – Population Health Re-Imagined
Healthcare organizations are increasingly using additional sources of data to augment their understanding and insights into the populations they serve, for a variety of purposes – from forecasting health outcomes and future use of services to development of strategies for outreach and engagement.
As good fortune would have it, the advent of electronic medical records and other home monitoring devices opens up new possibilities for incorporating relevant data about individuals under review within the health program evaluation framework.
Analytics for Population Health Management – Article 3 – May 2023
Accounting for Health Risk and Disease Prevalence
Population Health Management requires providers and program managers to maintain a delicate balance between taking a longer-term view of a target population (patient) experience and outcomes versus a short-term focus on individuals participating in a health management program and their near-term cost, utilization and outcomes. It is often difficult to see the forest for the trees, when too much of the analytic focus is centered around short-term experience, particularly when measured by cost and utilization results.
Analytics for Population Health Management – Article 2 – May 2023
Using a cost and utilization lens to evaluate and improve health care delivery
As interest in improving care management grows, it is important to establish which models of care are most effective. As described in our first article in this series on “Analytics for Population Health Management”, it has now been over ten years since the Institute for Healthcare Improvement (IHI) introduced the Triple Aim framework, which has served to ignite the realization that quality of care (done right) will not only improve patient experience, but also leads to improvements in overall population health and potential to reduce health care costs. The Triple Aim framework also served to highlight the unintended consequences of cost-cutting without an understanding of potential to put quality at risk. The IHI model represented the idea that evaluation of population health management programs and services should not simply look at cost drivers at the population level but must also take into consideration the drivers of individual level quality and outcomes. This article offers some perspective and suggestions for how to accomplish this.
Case Study – Leveraging Operational Data and Process Analytics for Efficient Delivery – March 2023
This case study outlines how to re-design a complex, high risk, end-to-end claims appeals intake to improve outcomes. The recommended re-design included metrics around timeliness and productivity, and Standard Operating Procedures (SOPs) to achieve a more streamlined and simplified organization and sustainable, improved performance. This goal was achieved through leveraging operational data and process analytics aimed at improving the effectiveness and efficiency of the medical claims appeals lifecycle.
Case Study – Managing with the Right Metrics – February 2023
Improving operational performance and delivery through identifying and measuring the key metrics, with a focus on aging and turnaround time, compliance, mitigating accreditation risk via new processes, reporting, and operational discipline.
Analytics for Population Health Management, Introduction to Series – January 2023
Maturing Analytics for Population Health Management
This is the first in a series of articles that will introduce an analytic capability and framework for translating health care data into actionable insights for population health management. Many healthcare organizations struggle to transform available data into viable solutions that improve patient care, while lowering cost of care at the same time. However, the growing emphasis on value-based healthcare has created the imperative for maturing analytics and unlocking insights needed to effectively manage population health and improve individual patient outcomes.
Primed Analytics Platform™ – November 2022
Primed Platform Supports Advanced Analytics Expectations of health care analytics platforms have evolved considerably over the past several years. While this is true for well-established organizations, startups also need to come to the table with a matured analytic capability out of the gate to compete in today’s fast moving and ever-changing business environment. Read More
Primed Analytics Platform – October, 2022
Evolving Health Care with Advanced Analytics Platforms
Expectations of health care analytics platforms have evolved considerably over the past several years for both start-ups and mature organizations. There is a growing need to accelerate the speed at which data is ready and available for business case development. Today’s fast moving, competitive environment calls for the ability to launch new initiatives quickly and be prepared to react proactively to rapidly changing market conditions.
Achieving Health Equity – August 2022
Achieving Health Equity – The focus has shifted to health payers and providers for solutions
U.S. public policy emphasis on Health Equity has been building for years. However, the COVID-19 pandemic and associated calls to action have now shifted attention to all parts of the health care system for potential solutions. The pandemic had a significant impact on the U.S. health and human services landscape, and inequities within the health care system propelled to the spotlight.
Lack of diversity in clinical trials isn’t just a recruiting problem—it’s a data problem
Leveraging the right data infrastructure and analytics can greatly improve healthcare processes. For example, though clinical trials have several obstacles to overcoming a lack of diversity, modernizing the data infrastructure and analytics is one of the most impactful improvements for such aspects as identifying the right patients to recruit. Modernizing also accommodates other improvements, such as:
- Identification of health inequity
- Root causes of disparity
As clinical trials are required to improve and pivot, so too is the way of wrangling the underlying diverse data streams and managing that data to present insights for better decision making in that recruitment process. DataWELL’s analytics and data platform are built for just that purpose, to support healthcare companies’ needs of:
- Speed of development
- Data management
- Leveraging one source of truth
- Timely data insights
“To achieve diversity goals in research requires a multifaceted approach that makes clinical trial participation easier and uses analytics to help identify the right patients to recruit for a clinical trial.” – Raj Indupuri (via MedCityNews.com)
(Links to a site external to DataWELL Informatics)
ANALYTIC INSIGHTS SERIES – Advancing Health Equity – May 2022
The WELL’s Analytic Insights Series provides generalizable knowledge derived from our analysis of acquired health care datasets, such as the CMS Medicare Data Set. The Insight Series represents the types of analyses we undertake in support of our clients and their business needs.
Our multi-disciplinary clinical, analytic, and technical team with a well-entrenched expertise in health care is uniquely equipped to zero in on fresh points of view. These viewpoints guide new directions in population health management at a variety of levels, such as health policy, product and business development, and improving clinical outcomes.
Advancing Health Equity
ANALYTIC INSIGHT SERIES – Next Level Care – April 2022
The WELL’s Analytic Insights Series provides generalizable knowledge derived from our analysis of acquired health care datasets, such as the CMS Medicare Data Set. The Insight Series represents the types of analyses we undertake in support of our clients and their business needs.
Our multi-disciplinary clinical, analytic, and technical team with a well-entrenched expertise in health care is uniquely equipped to zero in on fresh points of view. These viewpoints guide new directions in population health management at a variety of levels, such as health policy, product and business development, and improving clinical outcomes.
Telehealth after COVID
DERIVING VALUE: Planning for Payer Health Data
Healthcare’s continued transformation is driving further focus on utilizing a patient-centric approach. This approach requires a complete understanding of patient behaviors, needs, preferences, and outcomes. Payer health data is invaluable to unlocking essential insights into these patient aspects.
As you prepare initiatives using health payer data, several practical realities can stretch resources and timeframes beyond the initial plan. Having an awareness of the possible pitfalls will assists with setting more realistic expectations and may make a compelling case for seeking consultative services from experts with a solid track record in navigating these pitfalls
WEBINAR: DataWELL CEO, Rebecca Noreen Joins Panel to Discuss Virtual Care
Health insurance organizations are tasked with one of the greatest challenges of our era, ensuring the availability of quality, timely, cost-effective healthcare. With the experience of using virtual care during the pandemic, health plans are taking a fresh look at the efficiency, effectiveness, and accessibility of virtual care and seeing innovative uses, increased value and demand from patients and providers.
New reimbursement opportunities are paving the way for the future of virtual care.
This town hall panel discussion looks at how health insurance plans are using innovative technologies to assist in assuring coverage for their members while advancing workforce productivity.
CASE STUDY: Improving Patient Care Outcomes
Improving Patient Care Outcomes via combination of data sharing, provider relationship building, interactive peer level discussion, and clinical leadership training.
The Well partnered with a leading specialty clinical network to help improve patient outcomes through a combination of health care provider relationship building, improved data reporting, interactive education and discussion sessions, and clinical leadership training. The Well’s work paved the way for an expanded peer-to-peer clinical community for communicating best practices, fostering mutual trust, and sharing values. Providers including local clinic directors unanimously agreed that this approach had a positive impact on the practices, leading to improved outcomes.
Building Scalability: Part 3 – Technology
Timely and well-informed investments in new technology solutions are essential as drivers of performance and productivity, especially in the face of new business ventures and efforts to scale for associated growth. This is particularly true in the health care arena, where technology advancements are often the catalyst for shifting market opportunities – whether related to advancements in health care delivery, integration of new data sources, and/or proliferation of digital “wearable” home monitoring devices (Internet of Things). For example, the data that gets generated and stored from home monitoring devices such as glucose and blood pressure digital readers is available to be uploaded to electronic medical records and other databases for further analysis. However, this requires an infrastructure that supports integration from multiple sources.
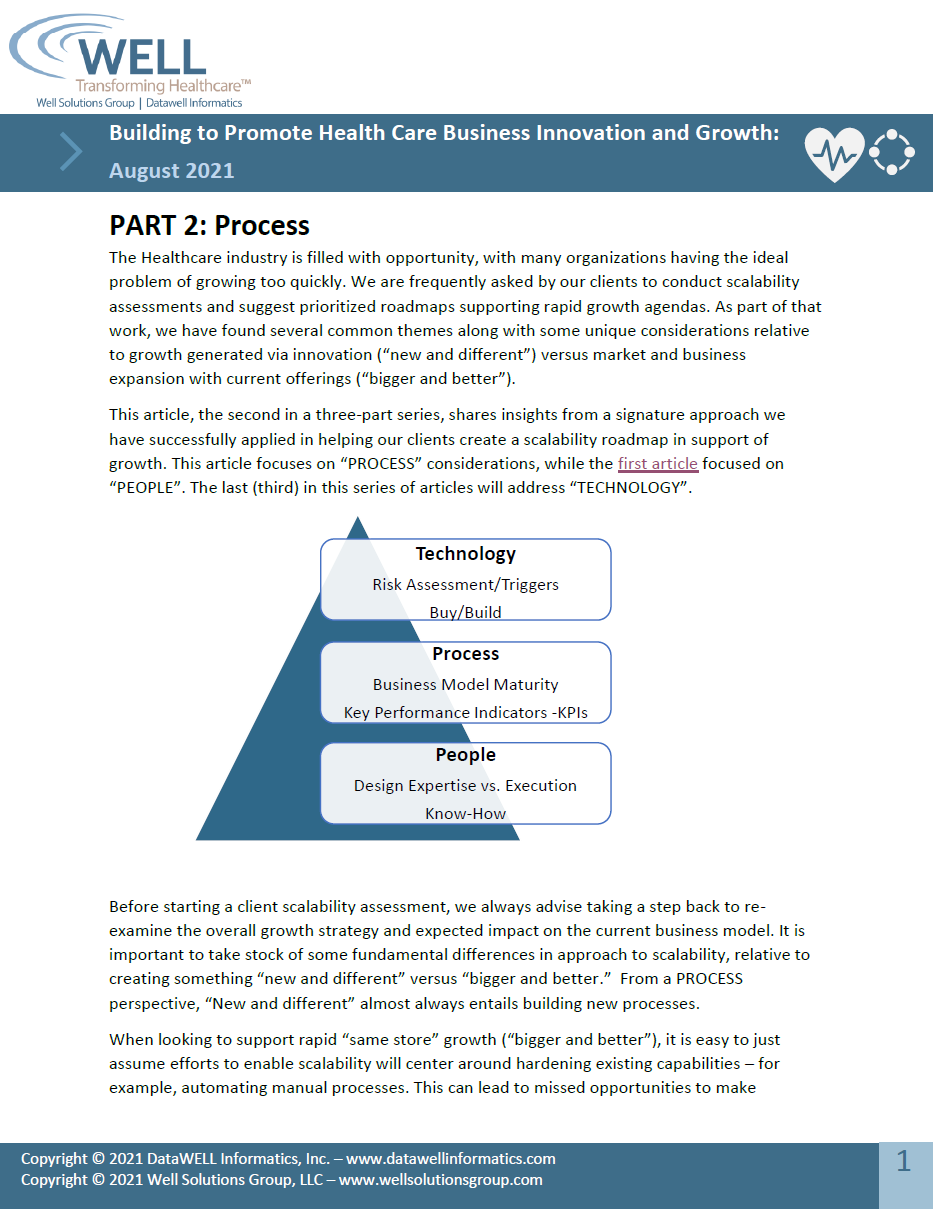
Building Scalability: Part 2 – Process
The Healthcare industry is filled with opportunity, with many organizations having the ideal problem of growing too quickly. We are frequently asked by our clients to conduct scalability assessments and suggest prioritized roadmaps supporting rapid growth agendas. As part of that work, we have found several common themes along with some unique considerations relative to growth generated via innovation (“new and different”) versus market and business expansion with current offerings (“bigger and better”).
Building Scalability: Part 1 – People
Health care organizations today need to factor scalability attributes into their business model(s) to stay abreast of a rapidly changing competitive environment, or risk being left behind. For a business to be scalable, it must focus on improving the profitability and efficiency of services even when its workload increases. However, establishing this capability does not occur in a vacuum and involves a complex set of considerations and analysis.
Identifying Seniors for Supplemental Benefits – Across the Health and Disease Continuum
COVID-19 pandemic has greatly exposed the critical importance of addressing the health-related social needs of vulnerable populations, especially older adults with complex medical conditions. Historically, single condition management programs have focused on one chronic disease, often missing opportunities to support other health care needs or interventions for primary prevention and health promotion. This represents a missed opportunity to engage Seniors in their own health and wellness activities by using additional benefits for services with greater impact on their overall health and conditions.
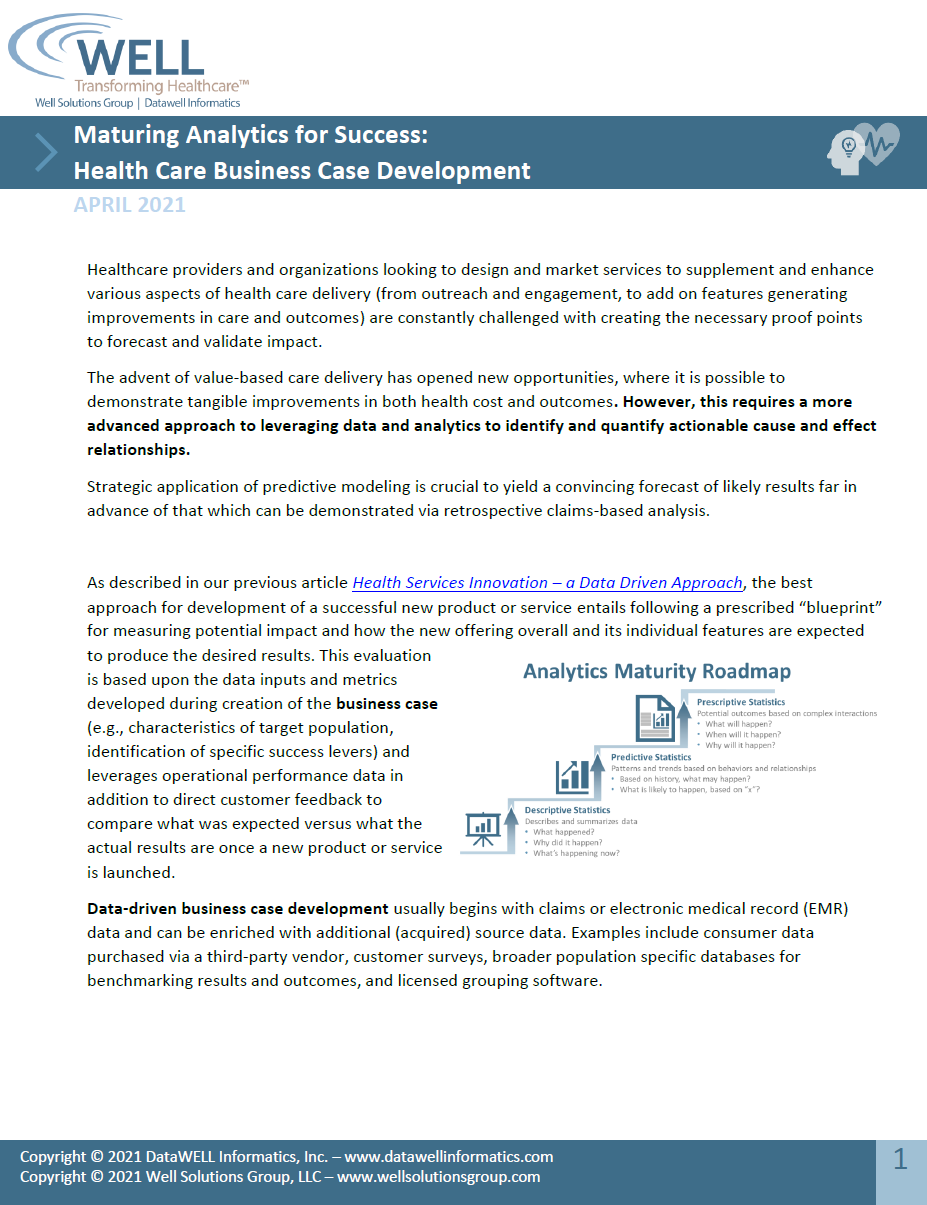
Maturing Analytics for Success:
Health Care Business Case Development
Healthcare providers and organizations looking to design and market services to supplement and enhance various aspects of health care delivery (from outreach and engagement, to add on features generating improvements in care and outcomes) are constantly challenged with creating the necessary proof points to forecast and validate impact.
The advent of value-based care delivery has opened new opportunities, where it is possible to demonstrate tangible improvements in both health cost and outcomes. However, this requires a more advanced approach to leveraging data and analytics to identify and quantify actionable cause and effect relationships.
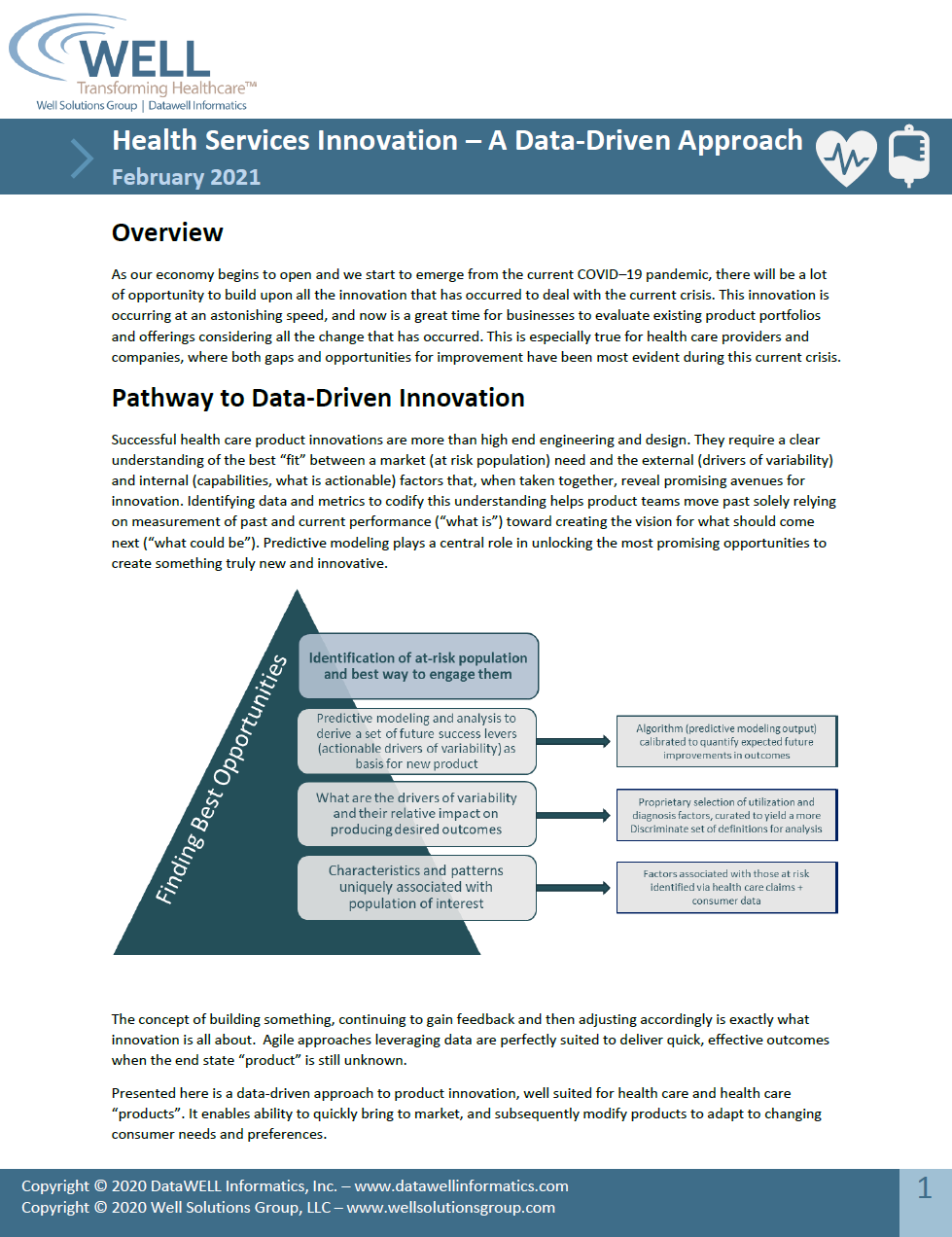
Health Services Innovation – A Data-Driven Approach
Successful health care product innovations are more than high end engineering and design. They require a clear understanding of the best “fit” between a market (at risk population) need and the external (drivers of variability) and internal (capabilities, what is actionable) factors that, when taken together, reveal promising avenues for innovation. Identifying data and metrics to codify this understanding helps product teams move past solely relying on measurement of past and current performance (“what is”) toward creating the vision for what should come next (“what could be”). Predictive modeling plays a central role in unlocking the most promising opportunities to create something truly new and innovative.
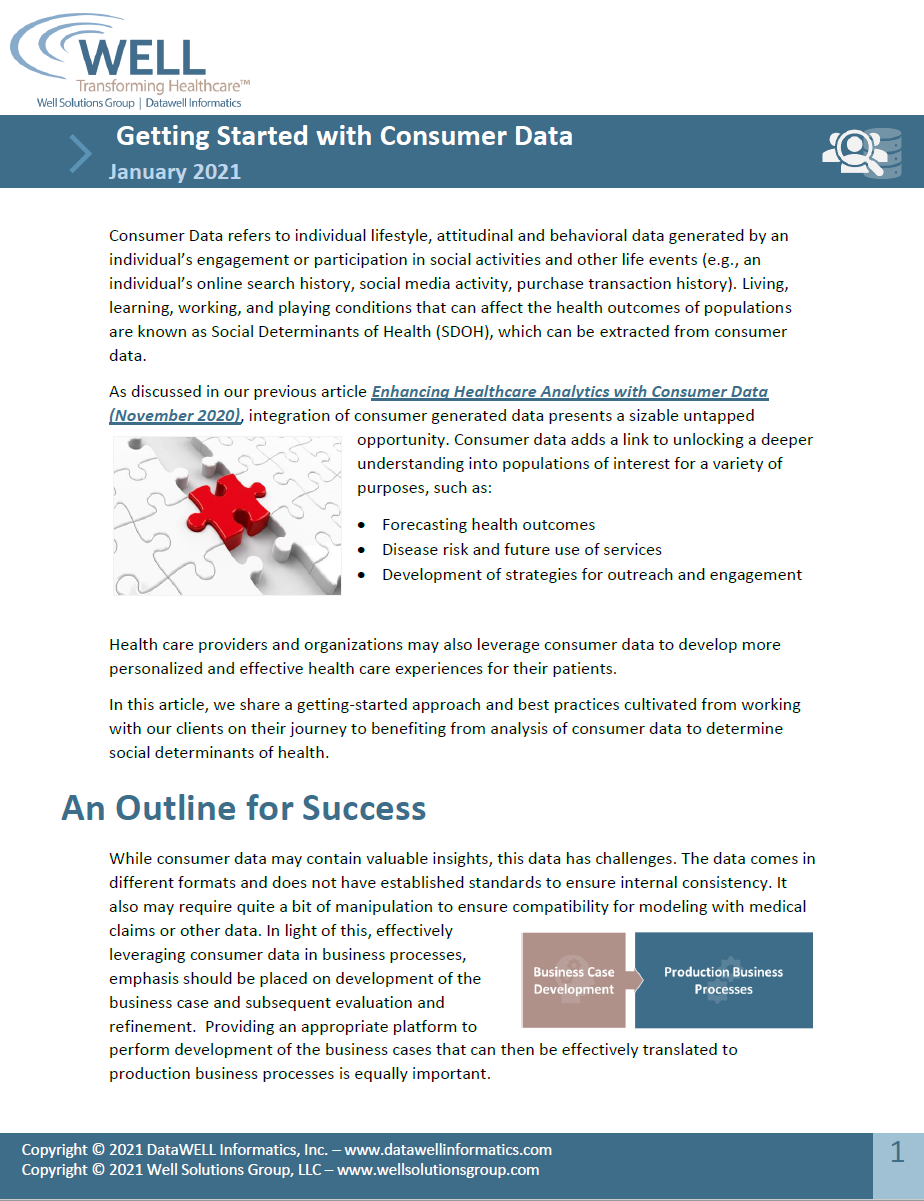
Getting Started with Consumer Data
Consumer Data refers to individual lifestyle, attitudinal and behavioral data generated by an individual’s engagement or participation in social activities and other life events (e.g., an individual’s online search history, social media activity, purchase transaction history). Living, learning, working, and playing conditions that can affect the health outcomes of populations are known as Social Determinants of Health (SDOH), which can be extracted from consumer data.
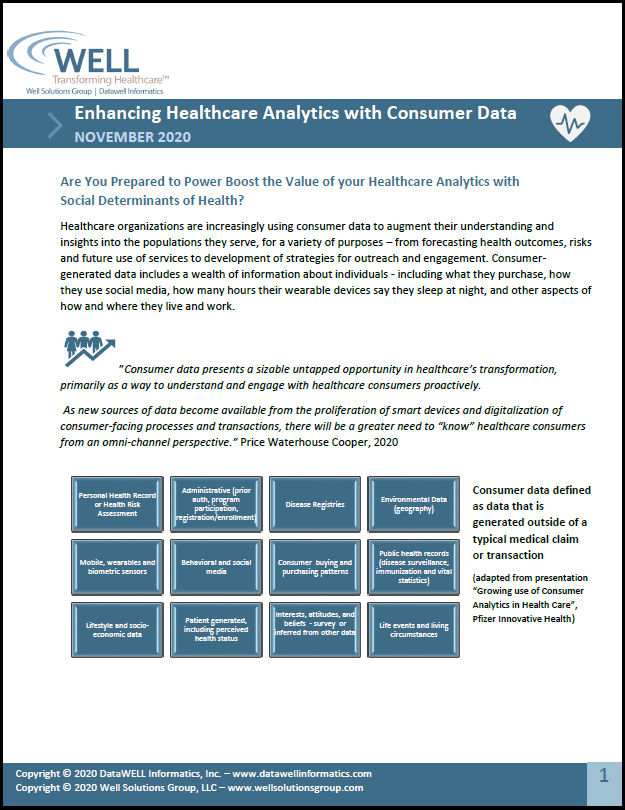
Enhancing Healthcare Analytics with Consumer Data
Healthcare organizations are increasingly using consumer data to augment their understanding and insights into the populations they serve, for a variety of purposes – from forecasting health outcomes, risks and future use of services to development of strategies for outreach and engagement. Consumer-generated data includes a wealth of information about individuals – including what they purchase, how they use social media, how many hours their wearable devices say they sleep at night, and other aspects of how and where they live and work.
Roadmap to Harnessing Value via Telehealth
Telehealth initiatives overall have shown potential to complement mainstream healthcare delivery at a lower cost and positive contribution to quality and outcomes (right care, right time).
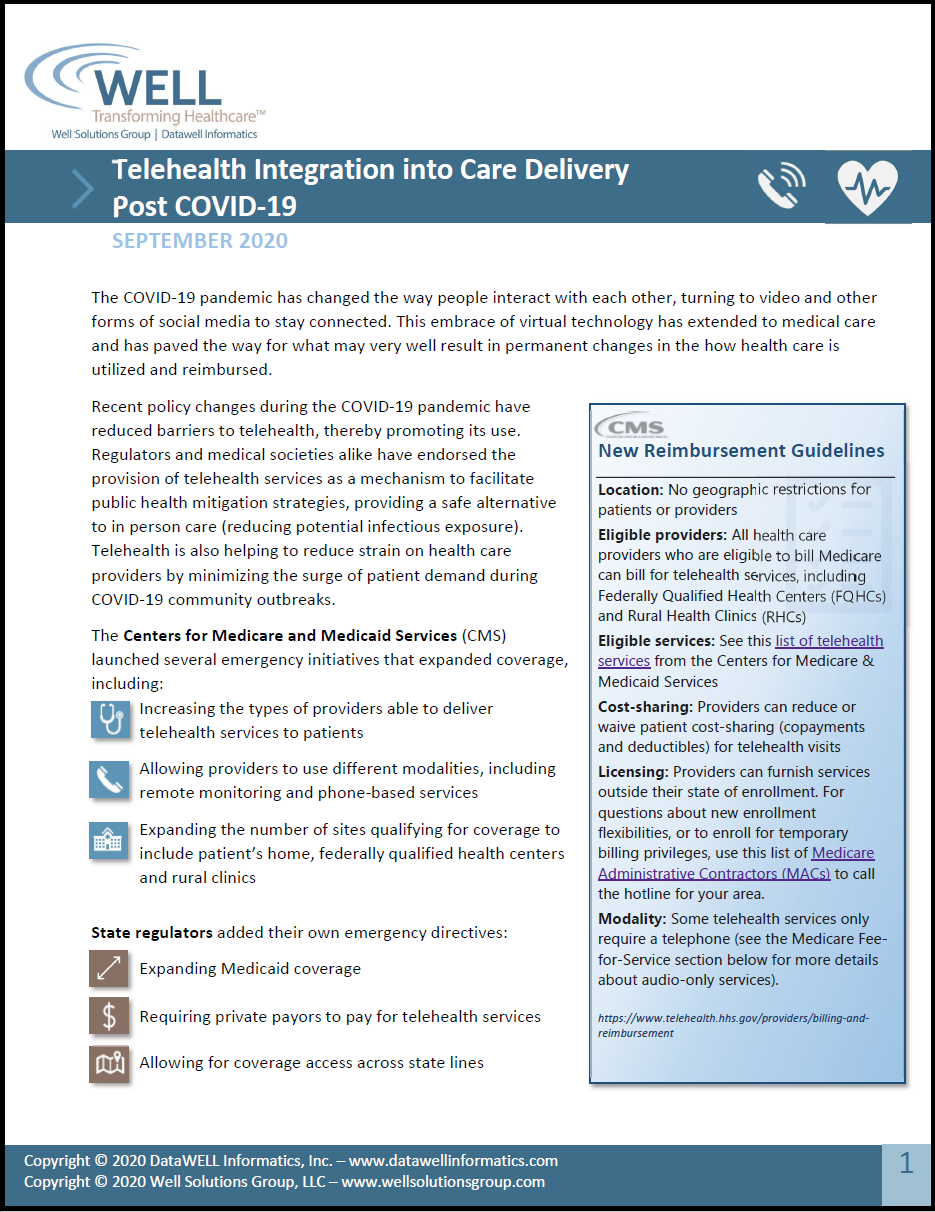
Telehealth Integration into Care Delivery Post COVID-19
The COVID-19 pandemic has changed the way people interact with each other, turning to video and other forms of social media to stay connected. This embrace of virtual technology has extended to medical care and has paved the way for what may very well result in permanent changes in the how health care is utilized and reimbursed.
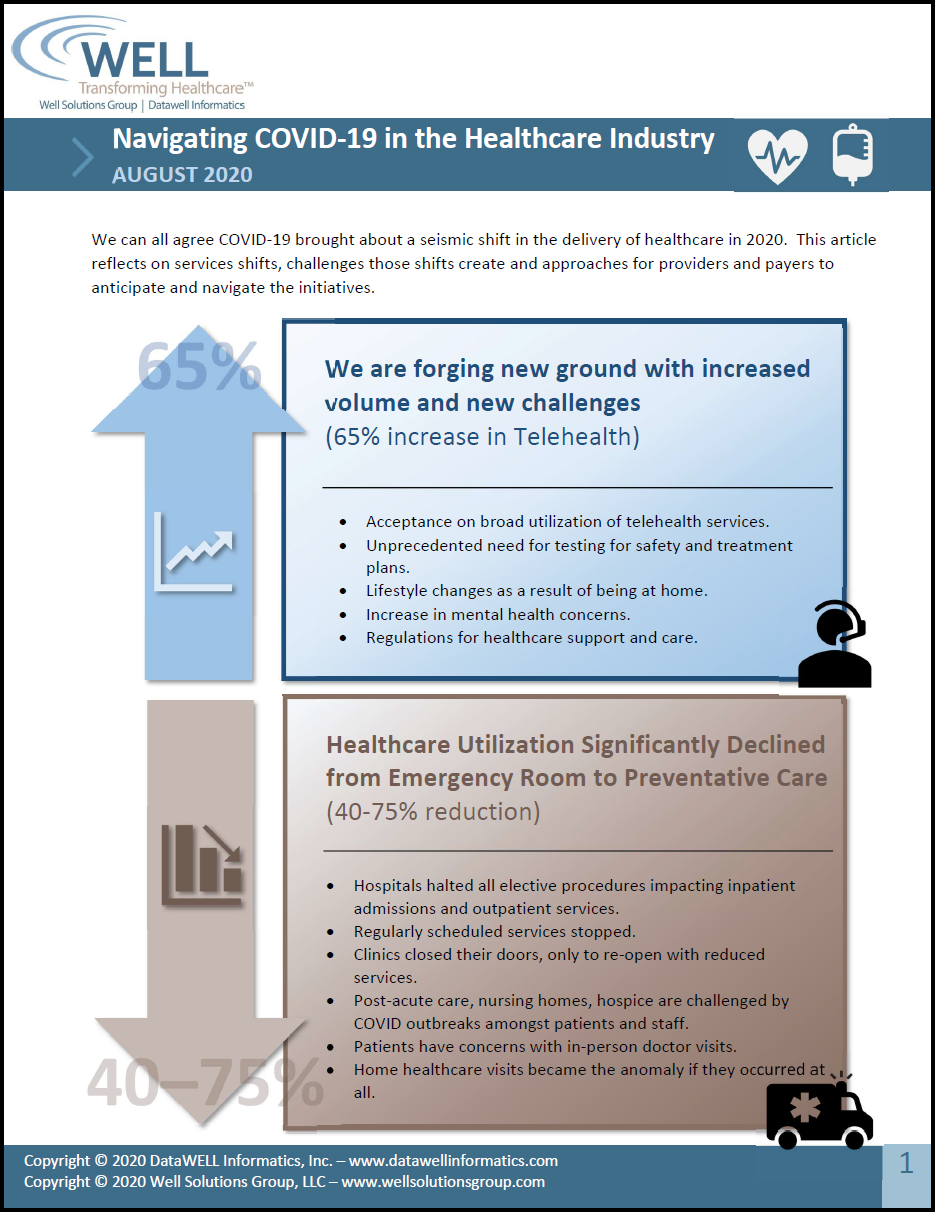
Navigating COVID-19 in the Healthcare Industry
We can all agree COVID-19 brought about a seismic shift in the delivery of healthcare in 2020. This article reflects on services shifts, challenges those shifts create and approaches for providers and payers to anticipate and navigate the initiatives.